New Challenges in Global Health

The Healthcare PPP Guide is designed to help high-level public- and private-sector executives engage in the design and execution of public-private partnerships. Though many in these kinds of roles are familiar with PPPs-some may have engaged with them in the past-PPPs still face significant capacity issues that limit their widespread use. Governments may feel they lack the highly-trained personnel necessary to pull off a PPP. They may feel ill-equipped to develop innovative solutions to complex problems, or unable to keep up with the breakneck pace of innovation emerging from the private sector. Conversely, the private-sector may feel less equipped to engage large numbers of citizens, or scale a project to address the needs of an entire country, for example. They may lack adequate funding. Or, even when a potent partnership opportunity presents itself, they may struggle to protect their bottom line while still delivering positive healthcare outcomes. The Guide is designed to help professionals in both sectors tackle all of these challenges and deliver solutions to the healthcare challenges facing a changing world.
With each passing year, the challenges facing Ministries of Health continue to mount, and 2020 has been no exception. As the world has developed since the millennium, so too have the diseases that we face. And while most Ministries of Health prepare to combat infectious diseases, many remain unprepared for the growing challenge of non-communicable diseases.
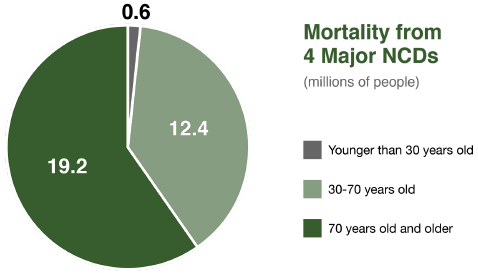
In the years prior to the Covid-19 pandemic, non-communicable diseases (NCDs) were responsible for 71 percent of global deaths. (Needless to say, with Covid-19 having claimed over one million lives as of this writing, that percentage will likely not hold.) The four major NCDs-diabetes, cardiovascular disease, chronic respiratory conditions, and cancer-kill 41 million people each year. (Chronic mental health conditions are also considered NCDs.) Of that 41 million, 15 million are considered premature, affecting individuals between 30 and 69 years of age; 85 percent of these premature deaths occur in low- and middle-income countries.2
Because they are chronic conditions, NCDs are incredibly difficult and expensive to manage. They strain healthcare structures-especially in rapidly-aging countries, where demand for healthcare and eldercare threatens to outpace supply, and in poorer countries, where a large percentage of the population cannot afford to pay a market rate for healthcare services.
What's more, the NCD crisis has now been imbued with an unfortunate new urgency. Covid-19 patients with preexisting NCD conditions are far more likely to become severely ill and suffer the most dire outcomes. Simply put, any strategy to address Covid-19-or prepare the world for future pandemics-must seek to address the growing problem of NCDs.
But while PPPs have been deployed in the past to great effect to combat infectious diseases like HIV/AIDS (and have even played a significant role in the Covid-19 crisis), they are only just beginning to play a role in the fight against NCDs. And while we can learn from the successes and failures of the fight against infectious disease to design PPPs for NCDs, the challenge of applying PPP models to NCDs is a complex one. The fight against NCDs will include efforts to improve both treatment and prevention, involving a wide variety of private-sector partners.
Furthermore, the global population continues to age, exacerbating the incidence and impact of these non-communicable diseases. Over 900 million people are elderly (defined as over the age of 60), and by 2050 that number is expected to rise to two billion, further straining our already-stretched healthcare and eldercare structures.3 Continuing urbanization creates economies of scale for hospital services (as citizens move closer to well-funded urban hospitals), but also exacerbates NCD risk factors (as citizens breathe polluted urban air or trade active, rural jobs for passive office work).
Massive structural and demographic issues like these present healthcare challenges. They present administrative challenges. And of course, they present humanitarian challenges. But they also present economic challenges-the challenge of delivering goods and services to people in need, the challenge of producing those goods and services affordably, and the challenge of creating economies of scale. In an ideal world, governments would be able to shoulder the massive costs associated with these kinds of issues, but unfortunately, they are often unable to address these issues alone. The scale of the challenge is simply too great, and the costs too high.
If we are to succeed in mitigating the effects of these diseases, governments and the private sector must be empowered and motivated to work together productively and sustainably. PPPs can be powerful tools for addressing complex public policy challenges like these.
Make no mistake: failure is a distinct possibility, and risk must be managed effectively. But, by leveraging the strengths of the public and private sectors at once, PPPs can deliver results where governments or the private sector alone might fail.
Once primarily considered financing tools, PPPs are increasingly being seen as catalysts for innovation. By leveraging the assets and capacity of both the public and private sectors, PPPs can deliver meaningful economic and social returns using collaborative solutions and governance.
___________________________________________________________________________________________________
2"Non-communicable diseases ," World Health Organization, 2018, https://www.who.int.
3 "Ageing and Health, "World Health Organization. 2018, https://www.who.int.